How much hydration or water do I actually need?
Should I pay for a hydration test?
How do I work out how much water/hydration I need when training?
Hydration is more of a marketing campaign than a scientific campaign – have you ever stopped to consider if you really need 8 to 10 glasses of water a day? This is the same myth and blunder as the recommendation of 10,000 steps a day. The magic number “10,000” dates back to a marketing campaign conducted shortly before the start of the 1964 Tokyo Olympic Games. A company began selling a pedometer called the Manpo-kei: “man” meaning 10,000, “po” meaning steps and “kei” meaning meter. It was hugely successful, and the number seems to have stuck.
There was also a marketing campaign in Japan to get people to drink more water and this is basically the American Colleges Sports Medicine position standpoint on hydration metrics and fluid guidelines across the board.
Elevated Plasma Volume
In a recent presentation by Dr. Stacy Sims, she discusses what you need to do to get your plasma volume elevated. There are some recommendations available via “web research” but they are not taking into account that there are specifically some sex differences in hormone pertubations that affect hydration and what us women need. You might ask why you need elevated plasma volume and the simple answer is successful adaptation through your training programme.
Dr Sims presented the information below, and what you might consider before deciding on your hydration strategy, is that there are sex differences in renal water and electrolyte retention. Many consider this subtle and probably not of consequence and this is really big misstep in a position stand. The science behind this has not really been reviewed and a critical eye taken to the science and studies that are out there specific to women.
The initial studies started way back in the 80s with Stephenson and Kolka, where they were looking at hydration parameters and thermal regulatory parameters in female soldiers so it is known that this information exists but it is not widely used nor implemented into the majority of hydration products or recommendations that you buy into.
It has been known for a very long time that there are sex differences between sweat rates, sodium losses, blood sodium levels at the end of exercise and finally someone has quantified it in a particular study just this year 2019[1]. From this study it is known that there are sex differences between total body sweat rates, like men sweat more than women, and although there are some women that do have greater sweat rates that can rival some men, but in general have a lower sweat rate.
Sweat rates are greater in the luteal phase[2], but it occurs at a later onset so when you are looking specifically at follicular versus luteal phase, there can be a little bit of a difference , but it’s that heat generation at the start that becomes the metric that most people are looking at.
It is also known that there are sweat sodium loss differences . Women lose way less sodium than men do in sweat. In the high hormone phase, we have less sweat sodium because across the board, our body has been kicking out more total body sodium and not retaining more, due to a switchover in our plasma osmolality ( plasma osmolality measures the body’s electrolyte-water balance ) and our hormones responsible for retaining sodium aldosterone, because progesterone and aldosterone compete for the same receptor site. When progesterone is elevated, aldosterone cannot tell the body to conserve more sodium so your body kicks out more.
(Aldosterone is the main mineralocorticoid hormone, is a steroid hormone produced by the zona glomerulosa of the adrenal cortex in the adrenal gland. It is essential for sodium conservation in the kidney, salivary glands, sweat glands and colon).
Our sweat sodium is lower in the luteal phase than it is in the follicular phase, so when you are looking across the two phases, and we know specifically that women have lower sweat sodium concentrations than men. When you look at total body sweat losses, this isn’t quite as large of a difference but there are still losses and total body sweat sodium losses, and this is dependent on where they collected the sweat which is why in this study there was no great difference because they used sweat patches in the same locations of the body. It is known that the type of sweating and the sweat onset are patterned differently across men’s bodies than women’s.
There is not a huge concern from Dr. Stacy that this is not quite so different but it’s very telling to know that sweat rates, and sweat sodium losses are different, because we are in that ubiquitous idea that women and men need to drink the same amount and you should use sodium tablets and you should use electrolyte tablets especially in long course racing, but AGAIN, this is driven more through marketing than science.
We know specifically that men and women have different hydration and sodium parameters. This is because of estrogen and progesterone, and estrogen is very specific to osmoregulation.
Note: A quality protein shake post training and cold tart cherry juice at night before bed also helps with rehydration.
It’s a pervasive idea that women and men need to drink the same amount and you should use sodium tablets, you should use electrolyte tablets, especially in long course racing but again this is driven more through marketing than actual science.
We know specifically that women have different hydration parameters to men. So if you think about why this is, estrogen, progesterone! Estrogen is very specific to osmoregulation. When you get too much “stuff” in your blood, your plasma osmolality comes up. When that comes up, it stimulates arginine vasopressin so you get the need to drink and rehydrate.
It stimulates your thirst, so when you get more concentration of stuff in your blood, you feel thirsty. You need more water in your blood and estrogen is tied tightly to that.
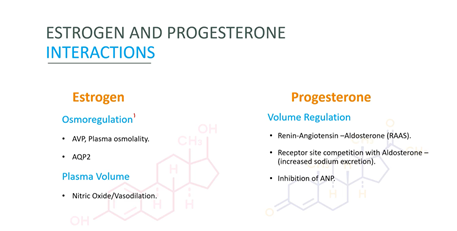
Slide Credit: Dr. Stacy Sims
The other aspect about estrogen is that it affects what is called the “aquaporin channel 2” in the kidney. This is what is responsible for that fluid shift of plasma volume out of the blood in the high hormone phase, because with greater estrogen, you have more permeability of fluid out of the blood to different spaces because of response in the kidney.
Refer to an article about beet juice (contains nitric oxide) which is not beneficial for females seeking training adaption, with the acute data on exercise indicating that it decreases VO2max and oxygen cost of exercise, you are actually losing training stimulus; elite athletes use it for this very reason- to reduce the cost of O2 use so they can go harder for longer in a race situation, but not when trying to garner training adaptations).[3]
We also know that estrogen is responsible for the whole nitric oxide vasodilation response, the more estrogen the more vasodilation, so women will vasodilate first before they start sweating. That’s a consideration you need to take into play when you think about how much hydration you need. Then think about progesterone which is more of a volume regulator. When you have constriction in the blood or a drop in your total blood or blood volume, it is a signal for your body to retain sodium. This is because sodium comes with water, and then we release aldosterone which is a slow response.
So it is a lag time really when you are thinking about rehydration. You need aldosterone to be secreted in order to allow your body to pull in more sodium and more fluid because both of these work together. So you have AVP and aldosterone working together to maintain that fluid balance. If you have high progesterone, you will have a reduction in aldosterone so if that happens your body will not receive the message to hold on to sodium so it kicks it out.
With elevated progesterone, your body kicks out more sodium which also drops plasma volume and that’s two-fold:
- Estrogen and its actions on the kidney
- Progesterone kicking out more sodium
The above two actions reduce plasma volume during high hormone phase.
It is known that hydration between the two hormone phase becomes very specific because we need to be thinking about what we are drinking in the high hormone phase to boost that plasma volume.
The low hormone phase doesn’t need such a careful metric but Dr. Stacy doesn’t advise being a little more lax (ie. pay attention still).
Oral Contraception
You have lower plasma osmolality for the AVP release. Think about what your estrogen is stimulating that arginine vasopressin, and it tightly controls your plasma osmolality (because it shifts across the phases)
So in your low hormone phase, your plasma osmolality is more elevated but your body doesn’t really stimulate the thirst as there is no drive to do that.
When you get into the high hormone phase with increased estrogen, and your plasma osmolality drops just by the nature of your threshold’s changing from estrogen, then the threshold drops and your thirst stimulus is not as strong as in the high hormone phase because you had that lower plasma osmolality.
So thinking about OC across the board with an elevation in estrogen, you already have lower plasma osmolality already because of the extra estrogen or that exogenous estrogen. and because you have that lower plasma osmolality as your baseline, then that means that your thirst sensation or the level to stimulate that arginine vasopressin release or that thirst, is lower. This is because your threshold is lower, so your threshold for thirst stimulation is lower, and the end result is less dehydration is required for fluid retention.
So that means that you need to think about your hydration metrics even more when you are on an OC. This also means you can’t compare with others who are not on OC as their hydration needs will be different.
So you have those considerations…
- You have to figure out what phase you are in -luteal or follicular?
- Do you need more sodium? Yes, in the high hormone phase
- You need more sodium just in your food, sprinkling it on your watery fruits and vegetables to allow your body to absorb more fluid and water.
- Does that mean you have to take salt tabs and electrolyte tablets on the course? NO.
Why? Because that is not a physiological mechanism for pulling sodium in. It causes more issues than it does benefit.
Thirst stimulation changes across the phases and also changes if you are on an OC. It is also known that with higher estrogen you have plasma osmolality that drops, and when you are in that lower range of plasma osmolality and keep drinking plain water, you’re at greater hyponaetremic risk.
It is also known that there are phase differences in your thermoregulatory thresholds. In the low hormone phase your thresholds allow you to tolerate more heat, and absorb more heat than when you are in the high hormone phase. You also have that shift in vasodilation in the high hormone phase and you start sweating and you sweat more, so that has to be taken into consideration too.
So considering all of these things now…. What do we do???
What Dr Stacy is saying is that you cannot programme your hydration into exactly x amount of fluid every 20 minutes, for example.
To figure out what you really need to do as an INDIVIDUAL is do your own test.

Slide Credit: Dr Stacy Sims
Look across the board at what you are doing for your own training.
Drink your usual hydration and use a urine dipstick that has a urine-specificity gravity (USG), and you want to see what happens with that USG change.
Start with your usual hydration and do a specific training session (ride, CrossFit, whatever) and the result of the test will be your baseline (Test A).
You want to measure your urine-specific gravity before and after training, and if it’s longer than 2 ½ hours and you have a pee in the middle of it, see what your USG is doing and see if your hydration drink is actually working for you. This could be tricky out in our desert, ladies!
Then a week later, do the same test but use a functional hydration drink (with no carb added and high in electrolyte) so that you’re actually absorbing that fluid and then compare the USG outcome on both tests.
You can also have a competition with your teammates and see who can wake up the most hydrated!
So the urine-specific dipstick is a really good way of determining how hydrated you are and what kind of things you need to do, as if you come out significantly dehydrated in test A and then you do all the recovery metrics and you believe you’re rehydrated, and then wake up the next morning and you’re still dehydrated then you going to get in a chronic state of dehydration or hypohydration, with slightly low body water that’s going to affect fatigue, recovery, cognition, and adaptations.
Then when you do test B, see what happens when you do a specific hydration intervention.
So that’s what you’re drinking, how often you’re drinking, and change it up and see.
What is your hydration metric at the end of test B, and then the next morning?
Stacy has a case study of a 70.3 athlete (because it’s more around that five hour race time mark!? – I wish…) and there are a lot of questions surrounding what happens in that longer endurance. Hydration becomes more of a focus metric of how to keep going without needing an urgent loo stop, without having GI distress, and how to hydrate well enough in the heat?
I don’t’ want to write the case study here… as I am still doing the course and also will write further about this when the course is complete. The above information has been typed out really quickly as I am listening to the presentation and there is a massive take away for me here below:
If you are going to have your hydration measured professionally, and they are not considering your hormonal phases or whether you are on oral contraception (or menopausal and on HRT (or both)), then perhaps consider not spending the money and do your own test as specified.
[1] https://www.ncbi.nlm.nih.gov/pubmed/31230518 J Sports Sci. 2019 Oct;37(20):2356-2366. doi: 10.1080/02640414.2019.1633159. Epub 2019 Jun 2
[2] https://www.ncbi.nlm.nih.gov/pubmed/25230913 Tohoku J Exp Med. 2014 Oct;234(2):117-22.
[3] https://www.facebook.com/drstacysims/photos/a.1726957927585575/2236163593331670/?type=3&comment_id=2236361633311866&reply_comment_id=2237160629898633&comment_tracking=%7B%22tn%22%3A%22R%2320%22%7D




